Whether it’s an orthopedic surgery or some other health event, you’re being discharged from the hospital. However, you aren’t quite ready to go home. Instead, you’ll be completing the next steps of your recovery journey in a nursing home for short-term rehabilitation. As if you don’t have enough on your mind, with all that your recovery entails, the last thing you should be worried about is who pays for this step.
Payment for Rehab Care: Facility Costs
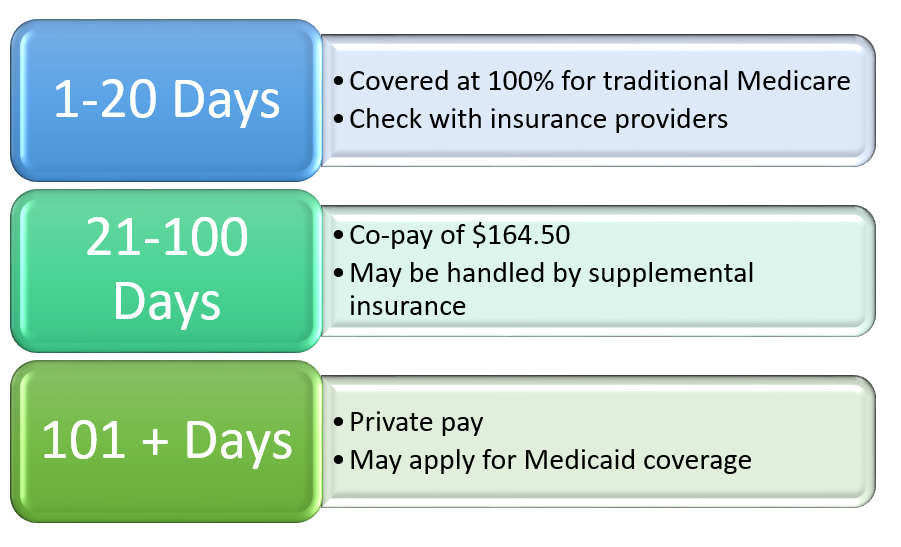
If you have a qualifying hospital stay,* you may be eligible for coverage for rehabilitation. Typically, the first 20 days in a rehabilitation facility should be covered at 100% through traditional Medicare A. According to Tom Millins, executive director at Cumberland Trace Health & Living, if you are not yet eligible for Medicare, you should check with your insurance provider as it will vary by insurance company and by your specific plan. He continued, “The hospital’s social workers and case managers can help you with this step because the hospital usually needs to get your insurance company to pre-approve your stay in rehab.”
Under Medicare, should your recovery last longer than 20 days, you then become responsible for co-pay. While that amount is determined annually by CMS (the government agency that handles Medicare), the current co-pay amount is $164.50 per day. This co-pay either comes out of your pocket, or it may be handled through your Medicare supplemental insurance. The co-pay amount remains in place for days 21-100 of rehabilitation services. For any days beyond 100, you move to a private pay status, responsible for all costs. If that is not feasible, you can apply for Medicaid coverage. Fortunately, most rehab stays last 30 days or less.
Payment for Rehab Care: Physician Costs
In addition to the costs of staying and receiving rehab services in a nursing home, you can expect physician charges that are separate from the facility charges. Typically, you will be seen in rehab less often than in the hospital. In fact, you may be seen only a few times during your stay, so these bills may be less than what you receive from hospital care.
*What is a Qualifying Hospital Stay?
All nights in the hospital are not the same. To become eligible for Medicare to pay for a rehab stay, a person must have 3 nights in the hospital as an INPATIENT. Time spent as an OBSERVATION patient does not count toward this 3 days. As a patient, it can be difficult to know if you are considered an inpatient or an observation patient because the bed you are in and the care you receive don’t necessarily change! If you want to know your status, ask your hospital case manager about this.
For additional information
Medicare has some links to explanations. Feel free to browse the website: https://www.medicare.gov/coverage/skilled-nursing-facility-care.html

No comments yet.